TMS for Stroke: A Breakthrough in Neurotherapy for Stroke Recovery
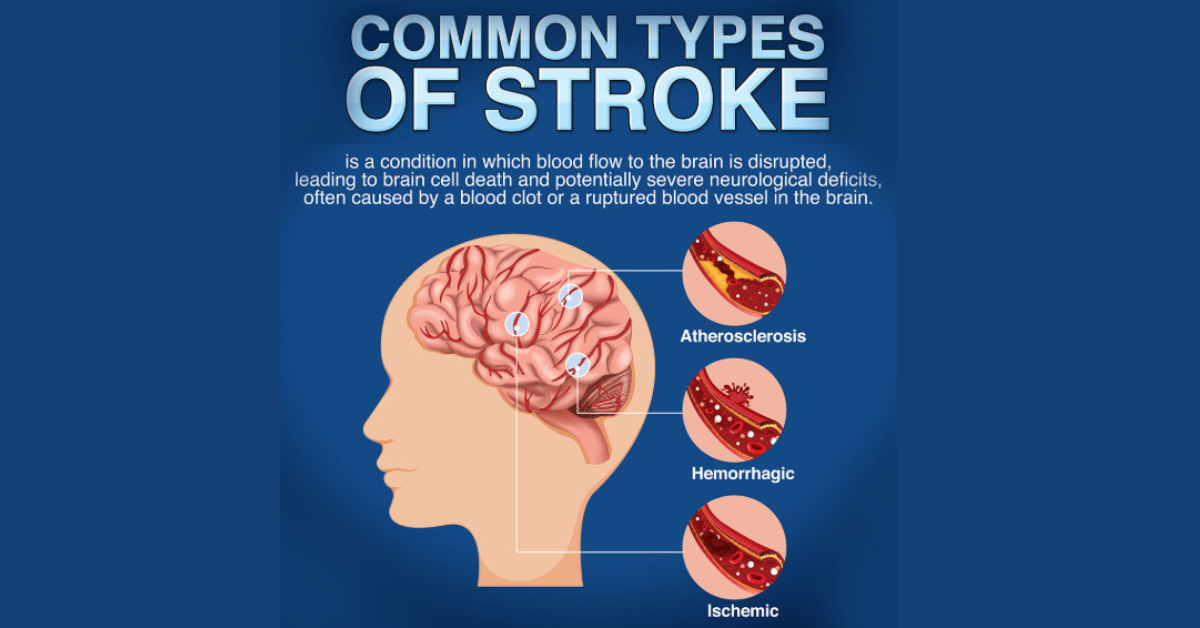
TMS For Stroke: Stroke is a life-altering condition that can significantly affect one’s motor skills, speech, and cognitive functions. While traditional rehabilitation therapies, such as physical therapy, speech therapy, and medications, offer varying degrees of recovery, a new therapy known as Transcranial Magnetic Stimulation (TMS) is emerging as an effective, non-invasive treatment option for stroke survivors. This blog explores how TMS, specifically TMS for stroke recovery, works and its potential benefits.
What is Transcranial Magnetic Stimulation (TMS)?
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate specific areas of the brain. Developed to treat mental health conditions like depression, TMS has gained traction in stroke rehabilitation due to its ability to promote brain plasticity—the brain’s ability to reorganize itself by forming new neural connections.
In the case of stroke, TMS targets brain areas that have been damaged and works to enhance recovery. The procedure involves using a magnetic device placed over the scalp to deliver pulses of electromagnetic energy into specific areas of the brain. These pulses stimulate neurons, promoting brain activity in regions that are often impaired after a stroke.
How TMS Can Help with Stroke Recovery
A stroke typically results in the interruption of blood flow to certain areas of the brain, leading to the loss of function in various parts of the body. TMS works by encouraging the brain to rewire itself, enabling damaged neural pathways to regenerate or strengthen existing ones. The therapy can:
-
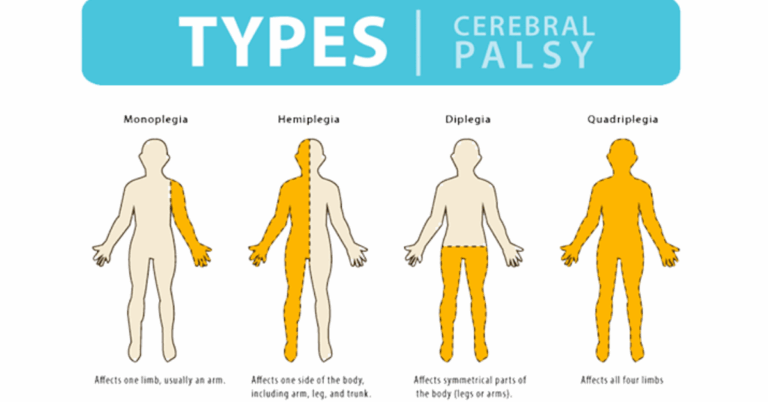
Improve Motor Function: One of the most common and debilitating effects of stroke is paralysis or weakness in limbs. TMS can stimulate the motor cortex, which controls voluntary muscle movements, helping to improve motor control and muscle strength.
-
Enhance Speech and Language Abilities: Many stroke survivors suffer from aphasia, a condition that affects speech and language. TMS can be used to stimulate areas of the brain responsible for language, such as Broca’s area and Wernicke’s area, promoting speech recovery.
-
Boost Cognitive Function: Stroke survivors may experience cognitive impairments, such as difficulty with memory, attention, or decision-making. By targeting regions involved in cognitive functions, TMS may help enhance these abilities.
-
Rehabilitate Brain Plasticity: By enhancing brain activity, TMS promotes neuroplasticity, which helps in repairing and rewiring damaged brain circuits. This ability is especially important in the recovery process post-stroke.
TMS for Stroke Recovery: The Therapy Process
TMS therapy for stroke is typically done in outpatient settings. The process generally involves the following steps:
-
Initial Assessment: Before starting therapy, a neurologist or a stroke specialist evaluates the patient’s condition. This includes understanding the extent of the stroke and identifying the specific areas of the brain that require stimulation.
-
Magnetic Pulse Delivery: During the procedure, a TMS machine is used to deliver targeted magnetic pulses to specific areas of the brain. The patient wears a cap or helmet that holds the magnetic coil in place. These pulses are non-invasive and painless, though some patients may feel mild discomfort.
-
Sessions: A typical TMS session lasts between 30-60 minutes, with multiple sessions scheduled over several weeks or months. The exact number of sessions varies based on the severity of the stroke and the patient’s response to treatment.
-
Post-Treatment Monitoring: After each session, the patient is monitored for any immediate side effects. Most patients can resume their daily activities right after the session without any issues.
Advantages of TMS for Stroke Rehabilitation
There are several advantages to using TMS as part of stroke rehabilitation:
-
Non-Invasive: Unlike surgeries or injections, TMS is a non-invasive therapy, making it a safe alternative for stroke patients.
-
Minimal Side Effects: TMS has few side effects, with some patients reporting mild headaches or discomfort during or after treatment. These side effects are generally temporary.
-
Accelerated Recovery: TMS therapy may speed up recovery in stroke patients, helping them regain lost functions more quickly compared to traditional rehabilitation methods.
-
Customized Treatment: TMS can be tailored to each patient’s unique needs. By focusing on specific brain areas, the therapy can be fine-tuned to target the deficits caused by the stroke.
TMS for Stroke: Research and Clinical Evidence
Numerous clinical studies have examined the effectiveness of TMS in stroke recovery. Research shows promising results, especially when the therapy is started soon after the stroke occurs. Some studies have reported improvements in motor skills, speech, and cognitive function after a series of TMS sessions.
In addition, TMS has been shown to work synergistically with other forms of rehabilitation, such as physical therapy and speech therapy, enhancing the overall effectiveness of the recovery process.
How TMS Stands Out in Stroke Recovery
Traditional stroke rehabilitation focuses on retraining the brain and body through physical exercises and therapies. While these therapies are essential, they do not directly stimulate brain regions that need recovery. TMS, on the other hand, directly influences the brain’s neural pathways, promoting recovery in a way that traditional therapies cannot.
Furthermore, TMS is particularly beneficial for patients who have not responded to conventional rehabilitation methods. For those with severe motor impairments or speech deficits, TMS may offer a new avenue of hope for recovery.
Frequently Asked Questions (FAQ)
1. Is TMS for stroke recovery safe? Yes, TMS is a safe procedure with minimal side effects. Most patients experience no adverse effects, though some may feel mild discomfort or headaches, which typically subside shortly after treatment.
2. How long does it take to see results from TMS therapy for stroke? Results can vary depending on the severity of the stroke and the individual’s response to the treatment. Some patients may begin noticing improvements after a few weeks, while others may take several months to see significant changes.
3. How many TMS sessions will I need? The number of sessions depends on the severity of the stroke and the patient’s individual needs. Typically, patients undergo 15-30 sessions over several weeks.
4. Can TMS be used for all types of strokes? TMS can be beneficial for many stroke patients, but it may be more effective when used shortly after the stroke. It is most commonly used for individuals who have experienced mild to moderate strokes.
5. Will TMS work if I had a stroke years ago? While early intervention is ideal, research has shown that TMS can still be beneficial for chronic stroke patients, even years after the stroke occurred. The therapy promotes brain plasticity, helping to rebuild neural connections.
6. Is TMS covered by insurance? Insurance coverage for TMS varies. Some insurance plans may cover the therapy for specific conditions, such as depression, but coverage for stroke rehabilitation may depend on the provider. It’s best to check with your insurance company for details.
Conclusion
TMS for stroke is an innovative, non-invasive treatment that holds great promise for improving recovery outcomes. As research continues to support its effectiveness, TMS therapy may become a key tool in the rehabilitation of stroke survivors, offering hope for better motor function, speech recovery, and cognitive improvement. If you or a loved one has experienced a stroke, consider exploring TMS as a potential treatment option to accelerate the healing process.